Magnesium for the Prevention & Treatment of Osteoarthritis-Induced Joint Pain
Do you have patients who present with or want to prevent joint pain? If so, this article could help you help your patients. Continue reading to learn more about a safe and clinically effective treatment option that is rarely prescribed for joint pain – magnesium! We are all familiar with the supplements most commonly prescribed to reliably support strong, healthy joints, such as collagen, omega-3 fatty acids, and anti-inflammatory botanical extracts, but what about magnesium?
Evidence suggests daily magnesium supplementation not only supports the maintenance of healthy joints but could also be beneficial to those who already have joint pain due to osteoarthritis (OA).
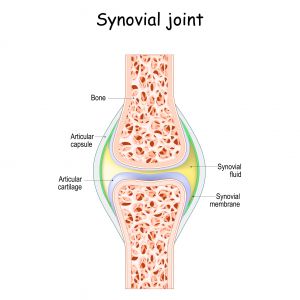
Anatomy Review – What is a Synovial Joint?
A joint is present in an area where two bones make contact. Joints are stabilized by muscles and include the connective tissue and bones. There are three main types of joints – fibrous, cartilaginous, and synovial. This article will focus on synovial joints, which include the elbow, knee, facet, and ankle joints.1
As you can see in the picture below, a healthy synovial joint includes bones, cartilage, and synovial membranes that produce synovial fluid.1
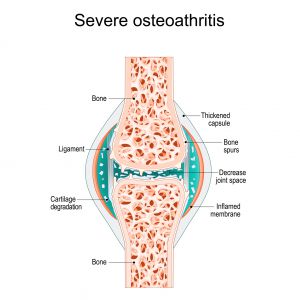
What is Osteoarthritis (OA)?
Osteoarthritis (OA) is the most common form of arthritis that affects the synovial joints. OA develops from gradual cartilage damage and thinning due to “wear and tear.” OA is more common in older than younger individuals and affects 14.8% of the global population older than 30 years of age.1,2
Approximately 595 million people were affected by OA globally in 2020, and over 1 billion individuals will have OA by 2050.2
The cartilage degradation process itself does not cause pain because the cartilage lacks nerves. The joint pain that does develop occurs due to the degradation and thinning of the cushioning cartilage, which then stimulates nerves in nearby areas to produce the pain signals. OA also causes the increased production of synovial fluid, leading to internal swelling, more pain, and stiffness. Eventually, OA can cause a very painful “bone on bone” condition. Bones have many nerves that can create excruciating pain signals as the cartilage degrades.1
The Clinical Association Between Low Magnesium Levels, Osteoarthritis (OA) & Joint Pain
Overall, the latest research demonstrates an inverse association between magnesium levels and the development of osteoarthritis (OA), which means those with more robust magnesium levels are less likely to develop OA.
A clinical study that included 2855 participants concluded that higher magnesium concentrations are associated with less radiographic evidence of OA in the knee.3 Another clinical study looked at the association between OA of the spine and magnesium levels. As in the knee, the presence of OA in the spine is significantly and directly correlated with a lower magnesium level in the blood.4
Cohort studies demonstrate a correlation between lower dietary magnesium intake, increased pain, and less function in the participants with knee OA. While several studies show a clear effect of magnesium status on OA, researchers have struggled to determine how magnesium beneficially affects joint health and patients with OA.3
How Does Magnesium Improve Joint Health and Control Osteoarthritis (OA) Joint Pain?
Animal studies show the injection of magnesium into a knee joint with OA relieves pain and slows down the development of cartilage damage. Research suggests the magnesium promotes the formation of new chondrocytes, which are the specialized cells that produce healthy cartilage.3 Evidence also suggests the magnesium injections stimulate the current chondrocytes to live longer and form new healthy cartilage within approximately two weeks.3,4
When researchers directly compared the injection of saline with the injection of magnesium into a synovial joint, they discovered the degree of cartilage degeneration was significantly lower after the injection of the magnesium.3 Magnesium is required for optimal cellular function and the production of cellular energy. In general, low magnesium levels induce a phenomenon known as cellular senescence, which is also known as biological aging.3
Magnesium Deficiency and Osteoarthritis (OA)-Associated Inflammation
Magnesium deficiency leads to elevated levels of inflammatory markers, including C-reactive protein, interleukin-6, NFκB, and tumor necrosis factor-α.5,6 The production of high levels of interleukin-6 is associated with the development of OA because animal studies show the inhibition of the interleukin-6 signaling pathway alleviates OA. Research shows magnesium directly inhibits the interleukin-6 signaling pathway in the cartilage and synovial tissues.5
A low magnesium level can also activate immune cells, including macrophages and neutrophils, to strengthen the inflammatory response. Therefore, low magnesium status could contribute to the development and progression of OA via inflammatory immune mechanisms. Magnesium deficiency is also associated with delayed bone differentiation and formation.5
Magnesium, Joint Health, and the Gut Microbiome
Researchers suspect magnesium could support healthy joints via its effects on the gut microbiome. Research shows low dietary magnesium intake leads to a reduction in beneficial bifidobacteria, which then increases systemic inflammation and triggers the development of OA. The loss of microbial diversity in the gut microbiome is also associated with increased frailty in elderly individuals.3
Researchers hypothesize the combination of probiotics, prebiotics, and magnesium could be a clinically effective therapeutic strategy for the prevention and treatment of OA.3
In summary, magnesium supports healthy joints by:
- Extending the lifespan of the cells that produce new, healthy cartilage
- Strengthening bones
- Inhibiting the destruction of cartilage
- Supporting healthy cellular function and cellular energy production
- Boosting the formation of new cartilage
- Modulating a healthy gut microbiome
- Slowing down cellular aging
- Reducing the production of inflammatory cytokines and neurotransmitters
- Alleviating pain3-5
The Best Magnesium Supplement Dose to Relieve Osteoarthritis (OA) Joint Pain
While research suggests magnesium supports healthy joints, too much of a good thing can be bad! Research shows the beneficial effects of magnesium do have an upper limit since excessive magnesium can inhibit cartilage formation.3 Fortunately, a cross-sectional study was conducted by Veronese et al. to determine the effects of a specific dose of magnesium on knee OA. The study determined a 100 mg increase in daily magnesium intake significantly boosted the cartilage volume and thickness of the knee joint surfaces in those with OA of the knee.7
The current Recommended Daily Allowance (RDA) for magnesium is 320 mg for non-pregnant women ages 31 and older. For men, the RDA for magnesium is 420 mg for ages 31 and older. Good sources of dietary magnesium include pumpkin seeds, almonds, cashews, black beans, and chia seeds. Magnesium supplementation can be prescribed if dietary intake is insufficient.8
Functional Laboratory Testing for Patients with Osteoarthritis (OA) Joint Pain
Both stress and magnesium deficiency are highly prevalent health concerns in modern times. Robust evidence shows that exposure to stressors is associated with lower blood magnesium concentrations and increased urinary excretion of magnesium.9
Since magnesium is required for and excreted during a healthy stress response, repeated or chronic exposure to stressors could significantly exacerbate the loss of magnesium and worsen the symptoms of OA and other health conditions if the magnesium is not replenished daily.10 Therefore, consider testing the urinary magnesium level with a Toxic Metals and Elements Panel to screen for excessive magnesium excretion in your patients with OA. The Adrenal Stress Index and Bone Health Panels are also indicated for all patients with osteoarthritis.

To place a test order, click here. As a reminder, DiagnosTechs will drop ship test kits directly to your patients, and you may select this option at the top of the order form.
Please visit our Provider Tools page for more information about choosing the right test, test result interpretation, and treatment options.
 References:
References:
- Juneja P, Munjal A, Hubbard JB. Anatomy, Joints. [Updated 2024 Apr 21]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507893/
- GBD 2021 Osteoarthritis Collaborators. Global, regional, and national burden of osteoarthritis, 1990-2020 and projections to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Rheumatol. 2023;5(9):e508-e522. doi:10.1016/S2665-9913(23)00163-7
- Kuang X, Chiou J, Lo K, Wen C. Magnesium in joint health and osteoarthritis. Nutr Res. 2021;90:24-35. doi:10.1016/j.nutres.2021.03.002
- Jakoniuk M, Kochanowicz J, Lankau A, et al. Concentration of Selected Macronutrients and Toxic Elements in the Blood in Relation to Pain Severity and Hydrogen Magnetic Resonance Spectroscopy in People with Osteoarthritis of the Spine. Int J Environ Res Public Health. 2022;19(18):11377. doi:10.3390/ijerph191811377
- Li G, Cheng T, Yu X. The Impact of Trace Elements on Osteoarthritis. Front Med (Lausanne). 2021;8:771297. doi:10.3389/fmed.2021.771297
- Pinto ACMD, de Melo Nunes R, de Freitas Carvalho WV, et al. Systemic and local antiinflammatory effect of magnesium chloride in experimental arthritis. Adv Rheumatol. 2024;64(1):6. doi:10.1186/s42358-023-00346-8
- Zhang Q, Yao Y, Chen Y, et al. A Retrospective Study of Biological Risk Factors Associated with Primary Knee Osteoarthritis and the Development of a Nomogram Model. Int J Gen Med. 2024;17:1405-1417. doi:10.2147/IJGM.S454664
- Office of dietary supplements – magnesium. NIH Office of Dietary Supplements. June 2, 2022. Accessed June 4, 2024. https://ods.od.nih.gov/factsheets/magnesium-healthprofessional/.
- Lopresti AL. The Effects of Psychological and Environmental Stress on Micronutrient Concentrations in the Body: A Review of the Evidence. Adv Nutr. 2020;11(1):103-112. doi:10.1093/advances/nmz082
- Pickering G, Mazur A, Trousselard M, et al. Magnesium Status and Stress: The Vicious Circle Concept Revisited. Nutrients. 2020;12(12):3672. doi:10.3390/nu12123672