
Cryptosporidiosis (Cryptosporidium Infection) – Symptoms, Diagnosis & Treatment
Cryptosporidium spp. (Crypto) is an intracellular protozoan parasite and a leading cause of diarrhea and mortality in immunocompromised individuals and young children across the globe.1-3 Crypto was initially recognized as a cause of diarrhea relatively recently, in 1976.3 Approximately 9% of mortality in children under the age of 5 globally is attributed to diarrheal diseases, including Crypto.4
An infection with Crypto is called cryptosporidiosis. According to serologic surveys, researchers suggest that an astounding 80% of North American adults have had cryptosporidiosis; however, most individuals likely do not know they have had a Crypto infection.5 As a single-celled parasite, Crypto is a member of the phylum Apicomplexa, which also includes the pathogens that cause toxoplasmosis and malaria.6
 Cryptosporidium (Crypto) – the Life Cycle of a Parasite
Cryptosporidium (Crypto) – the Life Cycle of a Parasite
Cryptosporidium occupies a unique intracellular niche at the brush border of the intestinal epithelial cells, where it undergoes a highly complex sexual life cycle. The complex life cycle renders Crypto difficult to culture and study. The entire life cycle unfolds in a single host, and all life cycle stages occur within a single cell type, the enterocytes of the small intestine.6
The life cycle of Crypto begins after the ingestion of a resilient, thick-walled oocyst, which contains four sporozoites. The change in temperature, gastrointestinal tract pH, proteases produced by the parasite, bile salt activity, and additional unknown triggering factors then facilitate the excystation of the sporozoites.1 After excystation, the sporozoites invade the epithelial cells that line the host organism’s small intestine. They transform into uninucleated trophozoites after invading the enterocytes.1,4
The sporozoites then undergo three rounds of merogony, an asexual replication, to produce a mature type I meront with eight merozoites. The released merozoites then invade adjacent enterocytes to produce additional type I meronts or transform into type II meronts with four merozoites.1
The merozoites from the type II meronts are thought to transform into the microgamont (male) and the macrogamont (female), which engage in sexual reproduction. The microgamont produces 16 bullet-shaped, non-flagellated male gametes that seek out the female for fertilization.1
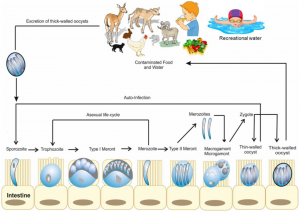
Image Source: Helmy YA, Hafez HM. Cryptosporidiosis: From Prevention to Treatment, a Narrative Review. Microorganisms. 2022;10(12):2456.
The fusion of the female and male nuclei after fertilization forms a diploid zygote that undergoes sporogony and meiosis to produce four haploid sporozoites within an oocyst that can be excreted in stool and taken up by another host to continue the life cycle.1 Unlike many other Apicomplexa that feature oocyst stages, the Crypto oocyst fully matures within the host cell and is infective immediately after release into the gut lumen.6
Asexual replication is predominant for up to 36 hours after infection, then there is a significant shift towards sexual reproduction. The microgamonts and macrogamonts begin to emerge 36 hours after infection and are abundant 48 hours after the initial infection with a Crypto oocyst.1 This timeline is consistent with the development of symptoms as soon as 2 days after infection.7
While the gastrointestinal tract is undoubtedly the principal site of infection and disease caused by Cryptosporidium, the frequency, extent, nature, and role of the respiratory tract in cryptosporidiosis need further investigation. Yes, evidence suggests that Crypto can be aspirated or inhaled into the lungs. Crypto might also be able to colonize and reproduce in the lungs and along other mucosal epithelial surfaces.8
 Cryptosporidium (Crypto) – Parasite Transmission
Cryptosporidium (Crypto) – Parasite Transmission
Cryptosporidium can cause infection via foodborne, zoonotic, waterborne, and human-to-human routes of transmission.3 Cryptosporidium hominis only infects humans, but Cryptosporidium parvum can infect and be transmitted by both humans and animals. Therefore, Cryptosporidium parvum is a prolific zoonotic pathogen.1
The oocysts of C. parvum are shed in large numbers in the feces of infected animals and humans.9 Crypto can also be transmitted via cough and the expectoration of oocysts during respiratory cryptosporidiosis.8 Crypto oocysts have thick walls and are robustly resilient during the metabolically dormant life cycle stage.4
The infectious oocysts are exceptionally resistant to chlorine and other disinfection procedures, which increases the difficulty when eliminating them from swimming pools and various environments.1 In fact, the oocysts can only be eliminated from water via filtration or boiling.9 Annually, oocyst resilience causes large outbreaks worldwide, including in developed countries. The outbreaks are often associated with recreational swimming facilities, such as community swimming pools, and the drinking water supply.1
 Crypto causes over half of the waterborne disease outbreaks associated with public hot tubs, swimming pools, and splash pads globally.2
Crypto causes over half of the waterborne disease outbreaks associated with public hot tubs, swimming pools, and splash pads globally.2
Moreover, a 2024 study tested for the presence of Crypto in pre-washed vegetables from supermarkets in the UK. The data showed that 58% of ready-to-eat vegetables were positive for Crypto. Further testing demonstrated that approximately 17% of the positive samples were contaminated with highly infectious C. parvum.9
Researchers speculate that oocysts are likely present in 65% – 97% of North American surface waters. An astounding 80% of North American adults have had cryptosporidiosis, according to serologic surveys; however, most individuals likely did not know they were infected with Crypto.5
 Symptoms of a Parasitic Cryptosporidium Infection (Cryptosporidiosis)
Symptoms of a Parasitic Cryptosporidium Infection (Cryptosporidiosis)
The infectious dose of Cryptosporidium oocysts is estimated to be as low as only 10 – 30 oocysts. Some researchers suggest that even a single oocyst can cause cryptosporidiosis, particularly in immunocompromised individuals.10 While some patients can experience an asymptomatic Cryptosporidium infection, symptoms tend to begin for most approximately 2 – 10 days (average of 7 days) after the initial infection with the oocyst(s).5,7 Symptoms often resolve within 2 – 3 weeks (with a range of a few days to 4 or more weeks) in immunocompetent patients. Gastroenteritis and other symptoms can be intermittent, typically for up to 30 days.7
Prolonged, frequent, and watery moderate to severe diarrhea is the most common symptom of cryptosporidiosis. Other common symptoms may include:
- Abdominal cramps, pain, or tenderness
- Dehydration
- Fever
- Nausea
- Vomiting
- Weight loss7
Patients who are immunocompromised due to immunosuppressive medications, HIV/AIDS, or genetic disorders, such as congenital hypogammaglobulinemia, can develop chronic illness and life-threatening sequelae.7 Children under 5 can also develop life-threatening disease. Cryptosporidiosis is the second most common cause of diarrhea-associated death in children between 12 and 23 months.9 Cryptosporidiosis primarily affects the small intestine in the gastrointestinal tract. However, in those with weakened immune systems due to HIV/AIDS or other conditions, cryptosporidiosis can affect the urinary bladder, the pulmonary system, and other areas of the digestive tract, including the pancreas and hepatobiliary tract.7,8
Less common signs, symptoms, and sequelae include:
- Acute pancreatitis11
- Anorexia8
- Cancer11
- Cognitive deficits4,9
- Cough8
- Death9,12
- Dizziness13
- Dyspnea8
- Eye discomfort13
- Failure to thrive and stunted growth in children and infants4,6,9
- Fatigue9,13
- Hemolytic Uremic Syndrome11
- Hypoxia8
- Inflammation of the nasal mucosa, sinuses, larynx, and trachea8
- Joint pain13
- Loss of Appetite11
- Malnutrition9,12
- Muscle weakness11
- Post-Infectious Irritable Bowel Syndrome (IBS)11,13
- IBS symptoms persist after complete recovery and parasite clearance, and protozoal enteritis shows the highest risk for PI-IBS development.13
- Reactive arthritis (Reiter’s Syndrome)11
- Recurring headaches9,13
- Rhinorrhea12
- Voice changes8
- Wheezing and crackles during lung auscultation12
Data from one study suggest that almost half of pediatric patients with a respiratory Cryptosporidium infection do not present with respiratory tract symptoms and likely have a lower, rather than an upper, respiratory tract colonization.12 Furthermore, numerous cases of respiratory cryptosporidiosis have been characterized by coinfections with other pathogens, including Mycobacterium, Pneumocystis jirovecii, and cytomegalovirus (CMV).8
Research also demonstrates that the evidence of causal links between cryptosporidiosis and colon cancer is growing, which highlights the need for the effective prevention and control of Crypto in communities.14
 Diagnosis of Cryptosporidiosis
Diagnosis of Cryptosporidiosis
The first step towards controlling and minimizing the number of Crypto outbreaks is a quick and accurate diagnosis. Unfortunately, no clinical gold-standard diagnostic test exists for acute cryptosporidiosis.15
While stool microscopy is the preferred diagnostic method for most parasitic infections and the current mainstay of Crypto diagnosis, it is considered by many to be a suboptimal test for cryptosporidiosis. However, it is possible to diagnose cryptosporidiosis via microscopy.16 Ideally, patients will submit at least three stool samples collected on different days for analysis.17
Molecular tests, such as Polymerase Chain Reaction (PCR) tests, are being developed. However, the oocysts are so resilient that even the PCR test is useless unless the thick wall of the oocyst is broken down to access the genetic material inside.10 While molecular diagnosis options are increasing, stool antigen testing that does not require the disruption of the oocyst wall is available and reliable.10 The Cryptosporidium stool antigen test offers impressive specificity and sensitivity.16
DiagnosTechs includes both tests – stool microscopy and the Cryptosporidium antigen test – with every GI Health Panel and Comprehensive Ova and Parasites Panel. Since Crypto is highly infectious and easily spread in a household or community environment, all close contacts of the infected individual should be tested and treated.
 Antiparasitic Treatment for Cryptosporidiosis
Antiparasitic Treatment for Cryptosporidiosis
Prevention is the best treatment. The prevention of a Crypto infection and outbreaks is especially critical due to the lack of reliable treatment options for human cryptosporidiosis.14 The preventive interventions below may be critically important for patients with advanced HIV or other health conditions that impede the optimal function of the immune system.
To prevent Cryptosporidium outbreaks and infections:
- Avoid contaminated food and water.
- Do not consume raw oysters.
- Maintain good hand hygiene by washing hands frequently.
- Community hot tubs, swimming pools, and splash pads could be contaminated. Avoid these environments. Do not swallow any water from public recreational facilities.
- Lakes, rivers, and saltwater beaches can be contaminated; avoid them.
- Municipal water supplies can be contaminated since oocysts survive in water at CDC-recommended chlorine levels (1–3 mg/L) and pH (7.2–7.8) for more than 10 days.
- During a “boil water advisory,” follow any of the options below:
- Boil water for at least 3 minutes.
- Use a submicron personal-use water filter that is NSF-certified
- Other safe hydration options include:
- Nationally distributed bottled water
- Canned carbonated soft drinks
- Frozen fruit concentrates
- Pasteurized drinks
- Remember that ice may also be a source of Cryptosporidium.
- 3% hydrogen peroxide is more effective than a standard bleach solution for sanitizing purposes
- Avoid exposure to fecal material.
- Wash all produce. Research suggests that the following techniques effectively remove Crypto from produce:
- Running water: Place the produce in a sieve (strainer) and rinse under a gentle stream of cold tap water for 1 minute, gently moving the sieve so that all produce is thoroughly rinsed. After rinsing, shake the sieve gently to remove excess water. This technique removes approximately 80% of Cryptosporidium parvum.
- Vinegar: Mix one part vinegar with three parts cold tap water in a bowl of sufficient size to cover the produce with the 1.75% acetic acid solution. Place the produce in the bowl and stir for 1 minute by hand, swishing the produce around in the bowl. Pour the bowl’s contents into a sieve and rinse under a gentle stream of cold water for 30 seconds. Shake gently to remove excess water. This technique removes approximately 90% of Cryptosporidium parvum.
- Salad spinner: Fill the salad spinner with cold water. Place the produce in the spinner “cage” and stir by hand for 1 minute. Lift the cage out of the bowl, empty the water, place the cage with produce back in the bowl, and spin for 10 seconds twice in alternate directions to remove excess water from the produce. This technique removes approximately 90% of Cryptosporidium parvum.18
- Consider combining all three techniques by adding vinegar to the salad spinner before processing the produce, and then thoroughly rinsing the produce under a gentle stream of cold tap water for 1 minute. This combined technique was not tested during the study cited above.
- Patients diagnosed with cryptosporidiosis should refrain from swimming for at least 2 weeks after the complete resolution of symptoms.19
- The CDC and the American Academy of Pediatrics suggest that following this recommendation will help prevent Cryptosporidium oocysts from being transmitted through recreational water.2
 At this time, there is no definitive evidence for a clinically effective pharmaceutical agent for the reliable management of cryptosporidiosis in immunocompetent and immunocompromised patients.19 Nitazoxanide is the only pharmaceutical approved for the treatment of cryptosporidiosis in immunocompetent patients by the US Food and Drug Administration (FDA), European Medicines Agency (EMA), and Pharmaceuticals and Medical Devices Agency (PMDA). Unfortunately, nitazoxanide is poorly efficacious in young, malnourished children and immunocompromised individuals.8,12,20
At this time, there is no definitive evidence for a clinically effective pharmaceutical agent for the reliable management of cryptosporidiosis in immunocompetent and immunocompromised patients.19 Nitazoxanide is the only pharmaceutical approved for the treatment of cryptosporidiosis in immunocompetent patients by the US Food and Drug Administration (FDA), European Medicines Agency (EMA), and Pharmaceuticals and Medical Devices Agency (PMDA). Unfortunately, nitazoxanide is poorly efficacious in young, malnourished children and immunocompromised individuals.8,12,20
One animal study suggests that nutritional interventions may reduce the severity of cryptosporidiosis. In the study, the administration of prebiotics and dietary fiber resulted in a less severe infection compared to the control group, which was fed a diet lacking fiber and no prebiotics.14 Furthermore, cryptosporidiosis can contribute to lactase deficiency; therefore, all patients should avoid milk products until symptoms resolve.19
It is also important to prevent dehydration and malnourishment in patients with diarrhea and vomiting. Regular oral rehydration with electrolytes and other nutrients is recommended unless IV rehydration is required. In some cases, an elemental diet or TPN could be medically necessary for patients who are malnourished or at risk of malnourishment. Ideally, patients with cryptosporidiosis should consume frequent, small amounts of foods that are low-fat, lactose-free, caffeine-free, high-fiber, and bland.19
Naturopathic and other treatment options are offered in your Provider Portal in the document: Cryptosporidium Treatment Protocols
Retest the stool at least 1 week after the completion of the treatment protocol if symptoms do not resolve. Longer courses of treatment might be needed in such cases. Persistent symptoms may also represent causes other than Cryptosporidium or reinfection due to poor hygiene and other factors.2
 The Best Laboratory Test Panels to Diagnose a Parasitic Infection
The Best Laboratory Test Panels to Diagnose a Parasitic Infection
DiagnosTechs is known as the laboratory that detects the parasites that other laboratories may miss!
Diagnose cryptosporidiosis with one of these test panels:
- Regular GI Health Panel™with GP3x and Calprotectin
- Expanded GI Health Panel™with GP3x and Calprotectin
- Comprehensive Ova and Parasites Panel
- Extended Comprehensive Ova and Parasites Panel
To place a test order, click here. DiagnosTechs will drop ship test kits directly to your patients. You may select this option at the top of the order form.
 References:
References:
- Pinto DJ, Vinayak S. Cryptosporidium: Host-Parasite Interactions and Pathogenesis. Curr Clin Microbiol Rep. 2021;8(2):62-67. doi:10.1007/s40588-021-00159-7
- Clinical Care of Crypto. Centers for Disease Control and Prevention. June 25, 2025. Accessed August 20, 2025. https://www.cdc.gov/cryptosporidium/hcp/clinical-care/index.html.
- Khalil IA, Troeger C, Rao PC, et al. Morbidity, mortality, and long-term consequences associated with diarrhoea from Cryptosporidium infection in children younger than 5 years: a meta-analyses study. Lancet Glob Health. 2018;6(7):e758-e768. doi:10.1016/S2214-109X(18)30283-3
- Rodrigues E, Pallett MA, Straker LC, et al. Cryptosporidium modifies intestinal microvilli through an exported virulence factor. Cell Host Microbe. 2025;33(5):719-730.e5. doi:10.1016/j.chom.2025.04.001
- Weir E. The cryptic nature of cryptosporidiosis. CMAJ. 2001;164(12):1743.
- Guérin A, Striepen B. The Biology of the Intestinal Intracellular Parasite Cryptosporidium. Cell Host Microbe. 2020;28(4):509-515. doi:10.1016/j.chom.2020.09.007
- Symptoms of Crypto. Centers for Disease Control and Prevention. June 16, 2025. Accessed August 27, 2025. https://www.cdc.gov/cryptosporidium/signs-symptoms/index.html.
- Sponseller JK, Griffiths JK, Tzipori S. The evolution of respiratory Cryptosporidiosis: evidence for transmission by inhalation. Clin Microbiol Rev. 2014;27(3):575-586. doi:10.1128/CMR.00115-13
- Suleiman AJ, Mavrides DE, Maxamhud S, et al. Presence of Cryptosporidium parvum in pre-washed vegetables from different supermarkets in South East England: A pilot study. Parasitol Res. 2024;123(6):230. doi:10.1007/s00436-024-08250-w
- Kosik-Bogacka D, Łanocha-Arendarczyk N, Korzeniewski K, et al. Cryptosporidium Infection in Adult Kidney Transplant Patients: A Systematic Review and Meta-Analysis. J Clin Med. 2024;13(21):6395. doi:10.3390/jcm13216395
- Carter BL, Chalmers RM, Davies AP. Health sequelae of human cryptosporidiosis in industrialised countries: a systematic review. Parasit Vectors. 2020;13(1):443. doi:10.1186/s13071-020-04308-7
- Iroh Tam PY, Chisala M, Nyangulu W, et al. Respiratory cryptosporidiosis in Malawian children with diarrheal disease. PLoS Negl Trop Dis. 2021;15(7):e0009643. doi:10.1371/journal.pntd.0009643
- Alsaady IM. Cryptosporidium and irritable bowel syndrome. Trop Parasitol. 2024;14(1):8-15. doi:10.4103/tp.tp_10_23
- Widmer G, Carmena D, Kváč M, et al. Update on Cryptosporidium: highlights from the Seventh International Giardia and Cryptosporidium Conference. Parasite. 2020;27:14. doi:10.1051/parasite/2020011
- Chalmers RM, Alexander C. Defining the diagnosis of cryptosporidiosis. Lancet Infect Dis. 2021;21(5):589-590. doi:10.1016/S1473-3099(20)30575-2
- O’Leary JK, Sleator RD, Lucey B. Cryptosporidium diagnosis and research in the 21stcentury. Food Waterborne Parasitol. 2021;24:e00131. doi:10.1016/j.fawpar.2021.e00131
- Clinical Testing and Diagnosis for Crypto. Centers for Disease Control and Prevention. May 27, 2025. Accessed September 5, 2025.
- Temesgen TT, Robertson LJ, Stigum VM, Tysnes KR. Removal of Parasite Transmission Stages from Berries Using Washing Procedures Suitable for Consumers. Foods. 2021;10(2):481. doi:10.3390/foods10020481
- Fabre V. Cryptosporidia: Johns Hopkins Abx Guide. Cryptosporidia | Johns Hopkins ABX Guide. March 5, 2023. Accessed August 27, 2025.
- Pane S, Putignani L. Cryptosporidium: Still Open Scenarios. Pathogens. 2022;11(5):515. doi:10.3390/pathogens11050515



