Test & Optimize Saliva Progesterone Levels for Pain Management
Test & Optimize Saliva Progesterone Levels for Pain Management
Progesterone is a fascinating hormone produced by the adrenal glands, reproductive organs, and brain in men and women.1 Yes – men need progesterone too, even though progesterone is often thought of as a female hormone required for a healthy pregnancy and optimal fertility. While progesterone is produced in the most robust amounts during pregnancy, progesterone is an important steroid hormone that supports optimal general health for everyone.2
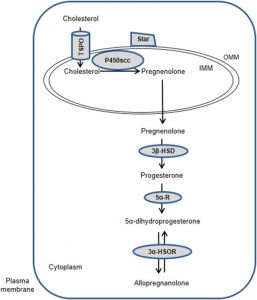
Progesterone is a sex hormone, and there are three classes of sex hormones – androgens, estrogens, and progestogens. Progesterone is one of the progestogen hormones.3 Like the other sex hormones, progesterone is derived from cholesterol after cholesterol is converted to the steroid hormone pregnenolone in the mitochondria.
 The Conversion of Cholesterol to Pregnenolone in the Mitochondria
The Conversion of Cholesterol to Pregnenolone in the Mitochondria
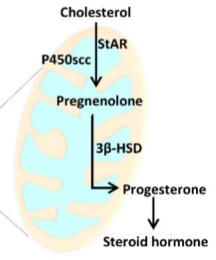 Image Source: Mitochondrial Function in Modulating Human Granulosa Cell Steroidogenesis and Female Fertility – PMC
Image Source: Mitochondrial Function in Modulating Human Granulosa Cell Steroidogenesis and Female Fertility – PMC
As a precursor for testosterone, estradiol, and other steroid hormones, progesterone is the most abundant hormone produced by the reproductive glands, and it affects fertility, immune function, pain management, bone health, and more.1,4 In women, progesterone is primarily synthesized by the corpus luteum in the ovary during the luteal phase of the menstrual cycle after ovulation, the adrenal glands daily, and the placenta during pregnancy.1
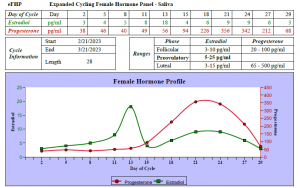
The red line in the graph below demonstrates the salivary progesterone levels present during an average optimal menstrual cycle:
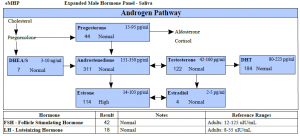
 In men, progesterone is predominately produced by the adrenal glands and testes and is a precursor for testosterone production.1
In men, progesterone is predominately produced by the adrenal glands and testes and is a precursor for testosterone production.1
Here is an illustration of the Androgen Pathway, which includes progesterone:
 Continue reading below to learn more about how an optimal salivary progesterone level affects natural opioid levels and pain management!
Continue reading below to learn more about how an optimal salivary progesterone level affects natural opioid levels and pain management!
 Progesterone and Pain Management
Progesterone and Pain Management
The medical literature currently acknowledges that progesterone and its metabolites are neuroprotective agents in the nervous system, demonstrating outstanding benefits in experimental models of Alzheimer’s disease, Parkinson’s disease, multiple sclerosis, and traumatic brain and spinal cord injuries.5 A significant and impressive number of studies have also determined that steroid hormones, particularly progesterone and its metabolite allopregnanolone, are implicated in the modulation of both neuropathic and nociceptive pain.5
Progesterone is a sex hormone that also acts as a neurosteroid since progesterone receptors are widely expressed throughout the nervous system.4 Research suggests that the nervous system synthesizes bioactive neurosteroids, including androgens, estrogens, and progesterone, either de novo from cholesterol or from circulating steroid hormone precursors. This process is known as neurosteroidogenesis. Remarkably, measurable levels of several neurosteroids are maintained in the brain and spinal cord despite the absence of adrenal and gonadal production.5
 How Do Steroid Hormones Affect the Nervous System?
How Do Steroid Hormones Affect the Nervous System?
There are multiple physiologic mechanisms by which progesterone and progesterone metabolites could be relevant to pain management. Steroid hormones exert effects in the nervous system by binding to intracellular/nuclear receptors to influence gene transcription and signaling pathways, influencing second-messenger pathways via membrane receptors, and modulating neuronal excitability via interaction with neurotransmitter receptors, including gamma-aminobutyric acid type A and N-methyl-D-aspartate receptors, L- and T-type calcium channels, and sigma-1 receptors.5
 The Impact of the Progesterone Metabolite Allopregnanolone on Pain Management
The Impact of the Progesterone Metabolite Allopregnanolone on Pain Management
Allopregnanolone is produced after progesterone is converted to 5α-dihydroprogesterone by the 5-α reductase enzyme. Research shows that allopregnanolone does not bind to the progesterone receptor. Rather, it regulates neuronal activity through its interaction with membrane receptors, including GABAA receptors and L- and T-type calcium channels. GABAA receptors and L- and T-type calcium channels are expressed in primary afferents and the sensory centers that control pain and nociception.5
The study of animal models of neuropathic pain has demonstrated a direct role of allopregnanolone in nociception and neuropathic pain. In both healthy and neuropathic animals, the knockdown or inhibition of allopregnanolone synthesis exerted a pronociceptive action. The pronociceptive effects are reversed by the direct intrathecal administration of allopregnanolone, confirm the physiologic impact of the allopregnanolone.5
 Neurosteroidogenesis – The Conversion of Cholesterol to Steroid Hormones in the Nervous System
Neurosteroidogenesis – The Conversion of Cholesterol to Steroid Hormones in the Nervous System
As depicted in this article, one rate-limiting step for neurosteroidogenesis is the shuttle of cholesterol into the inner mitochondrial membrane (IMM), which is mediated by the steroidogenic acute regulatory protein (StAR) and the 18 kDa translocator protein (TSPO).5
Once cholesterol is in the mitochondrion, the enzyme cytochrome P450 side-chain cleavage, located on the matrix side of the IMM, catalyzes the transformation of cholesterol into pregnenolone. Finally, the enzyme 3β-hydroxysteroid dehydrogenase (3β-HSD) converts pregnenolone to progesterone.5
Image Source: Allopregnanolone and Progesterone in Experimental Neuropathic Pain: Former and New Insights with a Translational Perspective
Neurosteroidogenesis Varies During Acute and Chronic Pain
Research suggests that an early activation of neurosteroidogenic pathways after an acute injury is a protective and endogenously regulated response that controls the development and transmission of pain.5
Unfortunately, during the chronic phase, neuroactive steroid production decreases in the peripheral and central nervous systems. Therefore, in chronic pain conditions, the increased local synthesis of protective steroids cannot be maintained, which likely contributes to abnormal sensory processing, the development of chronic pain, and pain severity.5
 The Administration of Progesterone for Pain Management – Clinical Evidence
The Administration of Progesterone for Pain Management – Clinical Evidence
Basic science and animal studies suggest a direct link between the local production of neurosteroids and the regulation of pain transmission.5 The currently available pharmaceutical treatment options for pain management have adverse side effects and poor efficacy. Therefore, the research and development of safe, new treatment options for pain management are crucial.5
Many studies have suggested that sex differences influence pain perception in men and women. Researchers speculate that pain perception might be different between men and women due to their varying levels of and responses to endogenous opioids and steroid hormones.4
Clinical studies in humans demonstrate that women are less sensitive to pain in the luteal phase of the menstrual cycle compared to the follicular phase. The luteal phase begins after ovulation when progesterone levels surge. Researchers describe the phenomenon as a state of “luteal analgesia,” during which there is a significant reduction in the emotional component of pain and reduced brain activation in response to painful stimuli.4
 The Impact of Progesterone on the Opioid System
The Impact of Progesterone on the Opioid System
The significant changes in hormone levels during pregnancy also appear to modulate the opioid system to reduce pain. Decreased pain sensitivity during pregnancy, or “pregnancy-induced analgesia,” has been demonstrated in many studies. Furthermore, an analysis of patients undergoing elective Caesarean section showed that higher progesterone levels correlated with lower pain levels during and after the surgery.4
Sex hormones, including progesterone, directly affect central opioid activity. Research shows that increased levels of progesterone trigger activation of the opioid system in the spinal cord, increase the natural release of endogenous opioids, and decrease sensitivity to pain. According to a study by Kondo et al., progesterone receptors in the central nervous system also play a role in developing neuropathic pain.4
Recent data suggest that bioidentical progesterone might increase the expression of delta-opioid receptors in the spinal cord and other areas to reduce pain. While changes in pain sensitivity and severity as a result of progesterone administration are still controversial, the research appears promising for pain management.4
Overall, there is an overwhelming amount of evidence that indicates progesterone and progesterone metabolites restore morphological, biochemical, and functional parameters after various types of peripheral nerve injuries due to chemotherapy, diabetes, physical trauma, and other causes to potentially mitigate the risk of developing chronic pain.5
 Functional Saliva Hormone Testing for Patients with Chronic Pain
Functional Saliva Hormone Testing for Patients with Chronic Pain
Patients with chronic pain could have low steroid hormone levels, including a low progesterone level. Low progesterone could be caused by dysfunction in the mitochondria, adrenal glands, and/or reproductive organs.1,5 Therefore, consider a customizable Flexi-MatrixTM panel that combines the Adrenal Stress Index with either the Expanded Male Hormone Panel or the Expanded Post Menopause Hormone Panel for your patients with chronic pain.
The Adrenal Stress Index and the Expanded Cycling Female Hormone Panel can be ordered as separate test panels for women with a menstrual cycle.
To place a test order, click here. As a reminder, DiagnosTechs will drop ship test kits directly to your patients.
Please visit our Provider Tools page for more information about Choosing the Right Test and Adrenal Restoration.
 References:
References:
- Bulletti C, Bulletti FM, Sciorio R, Guido M. Progesterone: The Key Factor of the Beginning of Life. Int J Mol Sci. 2022;23(22):14138. doi:10.3390/ijms232214138
- Nagy B, Szekeres-Barthó J, Kovács GL, et al. Key to Life: Physiological Role and Clinical Implications of Progesterone. Int J Mol Sci. 2021;22(20):11039. doi:10.3390/ijms222011039
- Pompili A, Iorio C, Gasbarri A. Effects of sex steroid hormones on memory. Acta Neurobiol Exp (Wars). 2020;80(2):117-128.
- Kolatorova L, Vitku J, Suchopar J, et al. Progesterone: A Steroid with Wide Range of Effects in Physiology as Well as Human Medicine. Int J Mol Sci. 2022;23(14):7989. doi:10.3390/ijms23147989
- González SL, Meyer L, Raggio MC, et al. Allopregnanolone and Progesterone in Experimental Neuropathic Pain: Former and New Insights with a Translational Perspective. Cell Mol Neurobiol. 2019;39(4):523-537. doi:10.1007/s10571-018-0618-1